Aden-Buie, Garrick. 2023.
“Epoxy: String Interpolation for Documents, Reports and Apps.” https://CRAN.R-project.org/package=epoxy.
Allaire, JJ, and Christophe Dervieux. 2024.
“Quarto: R Interface to ’Quarto’ Markdown Publishing System.” https://CRAN.R-project.org/package=quarto.
Altman, Douglas G, David Moher, and Kenneth F Schulz. 2017.
“Harms of Outcome Switching in Reports of Randomised Trials: CONSORT Perspective.” BMJ, February, j396.
https://doi.org/10.1136/bmj.j396.
Bengtsson, Henrik. 2024.
“Progressr: An Inclusive, Unifying API for Progress Updates.” https://CRAN.R-project.org/package=progressr.
Boutron, Isabelle, Douglas G. Altman, David Moher, Kenneth F. Schulz, and Philippe Ravaud. 2017.
“CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts.” Annals of Internal Medicine 167 (1): 40–47.
https://doi.org/10.7326/m17-0046.
Bradburn, Mike J., Ellen C. Lee, David A. White, Daniel Hind, Norman R. Waugh, Deborah D. Cooke, David Hopkins, Peter Mansell, and Simon R. Heller. 2020.
“Treatment Effects May Remain the Same Even When Trial Participants Differed from the Target Population.” Journal of Clinical Epidemiology 124 (August): 126–38.
https://doi.org/10.1016/j.jclinepi.2020.05.001.
Bryan, Jennifer, Craig Citro, and Hadley Wickham. 2023.
“Gargle: Utilities for Working with Google APIs.” https://CRAN.R-project.org/package=gargle.
Butcher, Nancy J., Andrea Monsour, Emma J. Mew, An-Wen Chan, David Moher, Evan Mayo-Wilson, Caroline B. Terwee, et al. 2022.
“Guidelines for Reporting Outcomes in Trial Reports.” JAMA 328 (22): 2252.
https://doi.org/10.1001/jama.2022.21022.
Calvert, Melanie, Jane Blazeby, Douglas G. Altman, Dennis A. Revicki, David Moher, Michael D. Brundage, and for the CONSORT PRO Group. 2013.
“Reporting of Patient-Reported Outcomes in Randomized Trials.” JAMA 309 (8): 814.
https://doi.org/10.1001/jama.2013.879.
Chamberlain, Scott, Hao Zhu, Najko Jahn, Carl Boettiger, and Karthik Ram. 2022.
“Rcrossref: Client for Various ’CrossRef’ ’APIs’.” https://CRAN.R-project.org/package=rcrossref.
Chess, Laura E, and Joel Gagnier. 2013.
“Risk of Bias of Randomized Controlled Trials Published in Orthopaedic Journals.” BMC Medical Research Methodology 13 (1).
https://doi.org/10.1186/1471-2288-13-76.
Corry, Ian S., Jonathan M. Webb, Amanda J. Clingeleffer, and Leo A. Pinczewski. 1999.
“Arthroscopic Reconstruction of the Anterior Cruciate Ligament.” The American Journal of Sports Medicine 27 (4): 444–54.
https://doi.org/10.1177/03635465990270040701.
Cumpston, Miranda, Tianjing Li, Matthew J Page, Jacqueline Chandler, Vivian A Welch, Julian PT Higgins, and James Thomas. 2019.
“Updated Guidance for Trusted Systematic Reviews: A New Edition of the Cochrane Handbook for Systematic Reviews of Interventions.” Cochrane Database of Systematic Reviews, October.
https://doi.org/10.1002/14651858.ed000142.
Fabricant, Peter D., Christopher M. Brusalis, Jonathan M. Schachne, Matthew J. Matava, Christian N. Anderson, Michael T. Busch, Henry G. Chambers, et al. 2020.
“Which Metrics Are Being Used to Evaluate Children and Adolescents After ACL Reconstruction? A Systematic Review.” Arthroscopy, Sports Medicine, and Rehabilitation 2 (4): e417–28.
https://doi.org/10.1016/j.asmr.2020.04.006.
Goldfeld, Keith, and Jacob Wujciak-Jens. 2020.
“Simstudy: Illuminating Research Methods Through Data Generation” 5: 2763.
https://doi.org/10.21105/joss.02763.
Haddaway, Neal R., Matthew J. Grainger, and Charles T. Gray. 2022.
“Citationchaser: A Tool for Transparent and Efficient Forward and Backward Citation Chasing in Systematic Searching.” Research Synthesis Methods 13 (4): 533–45.
https://doi.org/10.1002/jrsm.1563.
Hall, Kathryn T., Lene Vase, Deirdre K. Tobias, Hesam T. Dashti, Jan Vollert, Ted J. Kaptchuk, and Nancy R. Cook. 2020.
“Historical Controls in Randomized Clinical Trials: Opportunities and Challenges.” Clinical Pharmacology & Therapeutics 109 (2): 343–51.
https://doi.org/10.1002/cpt.1970.
Heathers, James. 2025.
“An Introduction to Forensic Metascience,” February.
https://doi.org/10.5281/ZENODO.14871843.
Hefti, E., W. Müller, R. P. Jakob, and H. -U. Stäubli. 1993.
“Evaluation of Knee Ligament Injuries with the IKDC Form.” Knee Surgery, Sports Traumatology, Arthroscopy 1 (3-4): 226–34.
https://doi.org/10.1007/bf01560215.
Hopewell, Sally, An-Wen Chan, Gary S Collins, Asbjørn Hróbjartsson, David Moher, Kenneth F Schulz, Ruth Tunn, et al. 2025.
“CONSORT 2025 Statement: Updated Guideline for Reporting Randomised Trials.” BMJ, April, e081123.
https://doi.org/10.1136/bmj-2024-081123.
Hopewell, Sally, Mike Clarke, David Moher, Elizabeth Wager, Philippa Middleton, Douglas G Altman, and Kenneth F Schulz. 2008.
“CONSORT for Reporting Randomised Trials in Journal and Conference Abstracts.” The Lancet 371 (9609): 281–83.
https://doi.org/10.1016/s0140-6736(07)61835-2.
Iannone, Richard, Joe Cheng, Barret Schloerke, Ellis Hughes, Alexandra Lauer, JooYoung Seo, Ken Brevoort, and Olivier Roy. 2024.
“Gt: Easily Create Presentation-Ready Display Tables.” https://CRAN.R-project.org/package=gt.
Janssen, Rob PA, Nicky van Melick, Jan BA van Mourik, Max Reijman, and Lodewijk W van Rhijn. 2017.
“Similar Clinical Outcome Between Patellar Tendon and Hamstring Tendon Autograft After Anterior Cruciate Ligament Reconstruction with Accelerated, Brace-Free Rehabilitation: A Systematic Review.” Journal of ISAKOS 2 (6): 308–17.
https://doi.org/10.1136/jisakos-2016-000110.
Jung, Lukas. 2024.
“Scrutiny: Error Detection in Science.” https://CRAN.R-project.org/package=scrutiny.
Junqueira, Daniela R, Liliane Zorzela, Susan Golder, Yoon Loke, Joel J Gagnier, Steven A Julious, Tianjing Li, et al. 2023.
“CONSORT Harms 2022 Statement, Explanation, and Elaboration: Updated Guideline for the Reporting of Harms in Randomised Trials.” BMJ, April, e073725.
https://doi.org/10.1136/bmj-2022-073725.
Kamatsuki, Yusuke, Marie Synnøve Qvale, Kathrin Steffen, Arnlaug Wangensteen, and Tron Krosshaug. 2024.
“Anatomic Risk Factors for Initial and Secondary Noncontact Anterior Cruciate Ligament Injury: A Prospective Cohort Study in 880 Female Elite Handball and Soccer Players.” The American Journal of Sports Medicine 53 (1): 123–31.
https://doi.org/10.1177/03635465241292755.
Khan, Mohammed Inayathulla, Inas Ismail, Savith Shetty, Jithin A Jebbar, Afra Faiaz, Shameez Mohammed, Abhishek V Shetty, Imthiaz Ahammed, and Mohammed Shahid. 2024.
“Functional Outcomes of Bone-Patellar Tendon-Bone Versus Quadrupled Semitendinosus and Gracilis Autografts for Anterior Cruciate Ligament Reconstruction.” Cureus, August.
https://doi.org/10.7759/cureus.66945.
Kilicoglu, Halil, Zeshan Peng, Shabnam Tafreshi, Tung Tran, Graciela Rosemblat, and Jodi Schneider. 2019.
“Confirm or Refute?: A Comparative Study on Citation Sentiment Classification in Clinical Research Publications.” Journal of Biomedical Informatics 91 (March): 103123.
https://doi.org/10.1016/j.jbi.2019.103123.
Kim, Haesook T. 2007.
“Cumulative Incidence in Competing Risks Data and Competing Risks Regression Analysis.” Clinical Cancer Research 13 (2): 559–65.
https://doi.org/10.1158/1078-0432.ccr-06-1210.
Liberati, Alessandro, Douglas G. Altman, Jennifer Tetzlaff, Cynthia Mulrow, Peter C. Gøtzsche, John P. A. Ioannidis, Mike Clarke, P. J. Devereaux, Jos Kleijnen, and David Moher. 2009.
“The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration.” PLoS Medicine 6 (7): e1000100.
https://doi.org/10.1371/journal.pmed.1000100.
Loo, M. P. J. van der. 2014.
“The Stringdist Package for Approximate String Matching” 6: 111–22.
https://CRAN.R-project.org/package=stringdist.
McCulloch, Peter, Douglas G Altman, W Bruce Campbell, David R Flum, Paul Glasziou, John C Marshall, and Jon Nicholl. 2009.
“No Surgical Innovation Without Evaluation: The IDEAL Recommendations.” The Lancet 374 (9695): 1105–12.
https://doi.org/10.1016/s0140-6736(09)61116-8.
McMillan, Lachlan B., and Lahann Wijenayake. 2024.
“The Top 100 Most Cited Articles in Australian Orthopaedic Surgery.” Journal of Orthopaedic Reports 3 (4): 100348.
https://doi.org/10.1016/j.jorep.2024.100348.
Migliorini, Filippo, Jörg Eschweiler, Yasser El Mansy, Valentin Quack, Markus Tingart, and Arne Driessen. 2020.
“Quadriceps Tendon Autograft for Primary ACL Reconstruction: A Bayesian Network Meta-Analysis.” European Journal of Orthopaedic Surgery & Traumatology 30 (7): 1129–38.
https://doi.org/10.1007/s00590-020-02680-9.
Moher, D., S. Hopewell, K. F Schulz, V. Montori, P. C Gotzsche, P J Devereaux, D. Elbourne, M. Egger, and D. G Altman. 2010.
“CONSORT 2010 Explanation and Elaboration: Updated Guidelines for Reporting Parallel Group Randomised Trials.” BMJ 340 (mar23 1): c869–69.
https://doi.org/10.1136/bmj.c869.
Nasreddine, Adam Y., Patricia L. Connell, Leslie A. Kalish, Susan Nelson, Maura D. Iversen, Allen F. Anderson, and Mininder S. Kocher. 2016.
“The Pediatric International Knee Documentation Committee (Pedi-IKDC) Subjective Knee Evaluation Form: Normative Data.” The American Journal of Sports Medicine 45 (3): 527–34.
https://doi.org/10.1177/0363546516672456.
Oussedik, Sam, Corey Scholes, Duncan Ferguson, Justin Roe, and David Parker. 2012.
“Is Femoral Component Rotation in a TKA Reliably Guided by the Functional Flexion Axis?” Clinical Orthopaedics & Related Research 470 (11): 3227–32.
https://doi.org/10.1007/s11999-012-2515-0.
Pinczewski, Leo A., David J. Deehan, Lucy J. Salmon, Vivianne J. Russell, and Amanda Clingeleffer. 2002.
“A Five-Year Comparison of Patellar Tendon Versus Four-Strand Hamstring Tendon Autograft for Arthroscopic Reconstruction of the Anterior Cruciate Ligament.” The American Journal of Sports Medicine 30 (4): 523–36.
https://doi.org/10.1177/03635465020300041201.
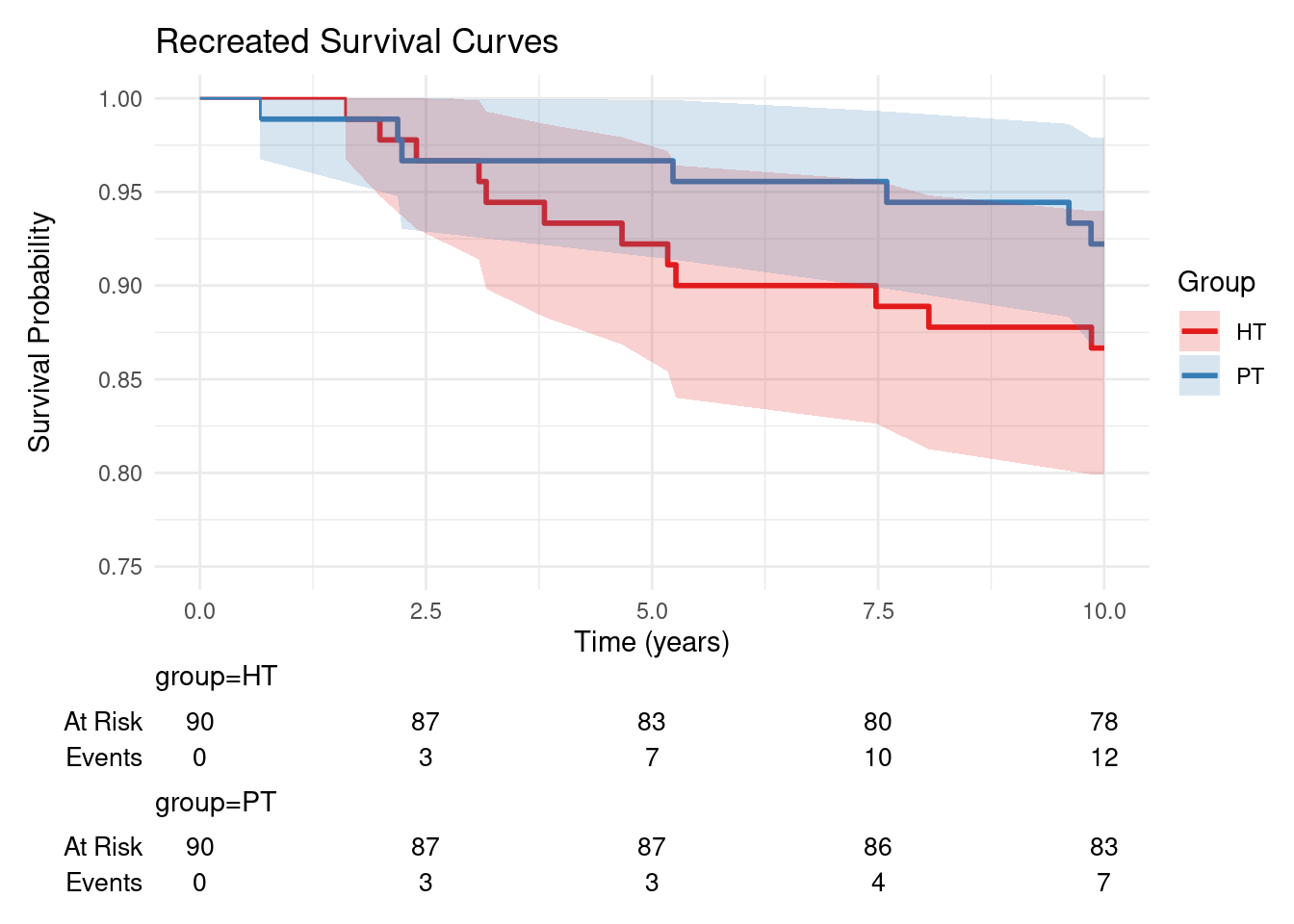
Pinczewski, Leo A., Jeffrey Lyman, Lucy J. Salmon, Vivianne J. Russell, Justin Roe, and James Linklater. 2007.
“A 10-Year Comparison of Anterior Cruciate Ligament Reconstructions with Hamstring Tendon and Patellar Tendon Autograft.” The American Journal of Sports Medicine 35 (4): 564–74.
https://doi.org/10.1177/0363546506296042.
R Core Team. 2024b.
“R: A Language and Environment for Statistical Computing.” https://www.R-project.org/.
———. 2024a.
“R: A Language and Environment for Statistical Computing.” https://www.R-project.org/.
Richardson, W. Scott, Mark C. Wilson, Jim Nishikawa, and Robert S. A. Hayward, eds. 1995.
“The Well-Built Clinical Question: A Key to Evidence-Based Decisions.” ACP Journal Club 123 (3): A12.
https://doi.org/10.7326/acpjc-1995-123-3-a12.
Rinker, Tyler W., and Dason Kurkiewicz. 2018.
“Pacman: Package Management for r.” http://github.com/trinker/pacman.
Roe, Justin, Leo A. Pinczewski, Vivianne J. Russell, Lucy J. Salmon, Tomomaro Kawamata, and Melvin Chew. 2005.
“A 7-Year Follow-up of Patellar Tendon and Hamstring Tendon Grafts for Arthroscopic Anterior Cruciate Ligament Reconstruction.” The American Journal of Sports Medicine 33 (9): 1337–45.
https://doi.org/10.1177/0363546504274145.
Rothman, K. J., J. E. Gallacher, and E. E. Hatch. 2013.
“Why Representativeness Should Be Avoided.” International Journal of Epidemiology 42 (4): 1012–14.
https://doi.org/10.1093/ije/dys223.
Rousseau, Romain, Charlotte Labruyere, Charles Kajetanek, Olivia Deschamps, Konstantinos G. Makridis, and Patrick Djian. 2019.
“Complications After Anterior Cruciate Ligament Reconstruction and Their Relation to the Type of Graft: A Prospective Study of 958 Cases.” The American Journal of Sports Medicine 47 (11): 2543–49.
https://doi.org/10.1177/0363546519867913.
Salika, Theodosia, Rebecca M. Turner, David Fisher, Jayne F. Tierney, and Ian R. White. 2022.
“Implications of Analysing Time-to-Event Outcomes as Binary in Meta-Analysis: Empirical Evidence from the Cochrane Database of Systematic Reviews.” BMC Medical Research Methodology 22 (1).
https://doi.org/10.1186/s12874-022-01541-9.
Schulz, Kenneth F, Douglas G Altman, and David Moher. 2010.
“CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials.” BMC Medicine 8 (1).
https://doi.org/10.1186/1741-7015-8-18.
Schuster, Noah A., Emiel O. Hoogendijk, Almar A. L. Kok, Jos W. R. Twisk, and Martijn W. Heymans. 2020.
“Ignoring Competing Events in the Analysis of Survival Data May Lead to Biased Results: A Nonmathematical Illustration of Competing Risk Analysis.” Journal of Clinical Epidemiology 122 (June): 42–48.
https://doi.org/10.1016/j.jclinepi.2020.03.004.
Sjoberg, Daniel D., Mark Baillie, Charlotta Fruechtenicht, Steven Haesendonckx, and Tim Treis. 2024.
“Ggsurvfit: Flexible Time-to-Event Figures.” https://CRAN.R-project.org/package=ggsurvfit.
Sjoberg, Daniel D., Karissa Whiting, Michael Curry, Jessica A. Lavery, and Joseph Larmarange. 2021.
“Reproducible Summary Tables with the Gtsummary Package” 13: 570–80.
https://doi.org/10.32614/RJ-2021-053.
Sollberger, V. D., A. Korthaus, A. Barg, and G. Pagenstert. 2022.
“Long-Term Results After Anterior Cruciate Ligament Reconstruction Using Patellar Tendon Versus Hamstring Tendon Autograft with a Minimum Follow-up of 10 Yearsa Systematic Review.” Archives of Orthopaedic and Trauma Surgery 143 (7): 4277–89.
https://doi.org/10.1007/s00402-022-04687-9.
TEGNER, YELVERTON, and JACK LYSHOLM. 1985.
“Rating Systems in the Evaluation of Knee Ligament Injuries.” Clinical Orthopaedics and Related Research 198 (&NA;): 42???49.
https://doi.org/10.1097/00003086-198509000-00007.
The ACL Registry Trust. 2024.
“New Zealand ACL Registry Annual Report 2024,” December.
https://www.aclregistry.nz/reports/.
Therneau, Terry M. 2024.
“A Package for Survival Analysis in r.” https://CRAN.R-project.org/package=survival.
Vaughan, Davis, and Matt Dancho. 2022.
“Furrr: Apply Mapping Functions in Parallel Using Futures.” https://CRAN.R-project.org/package=furrr.
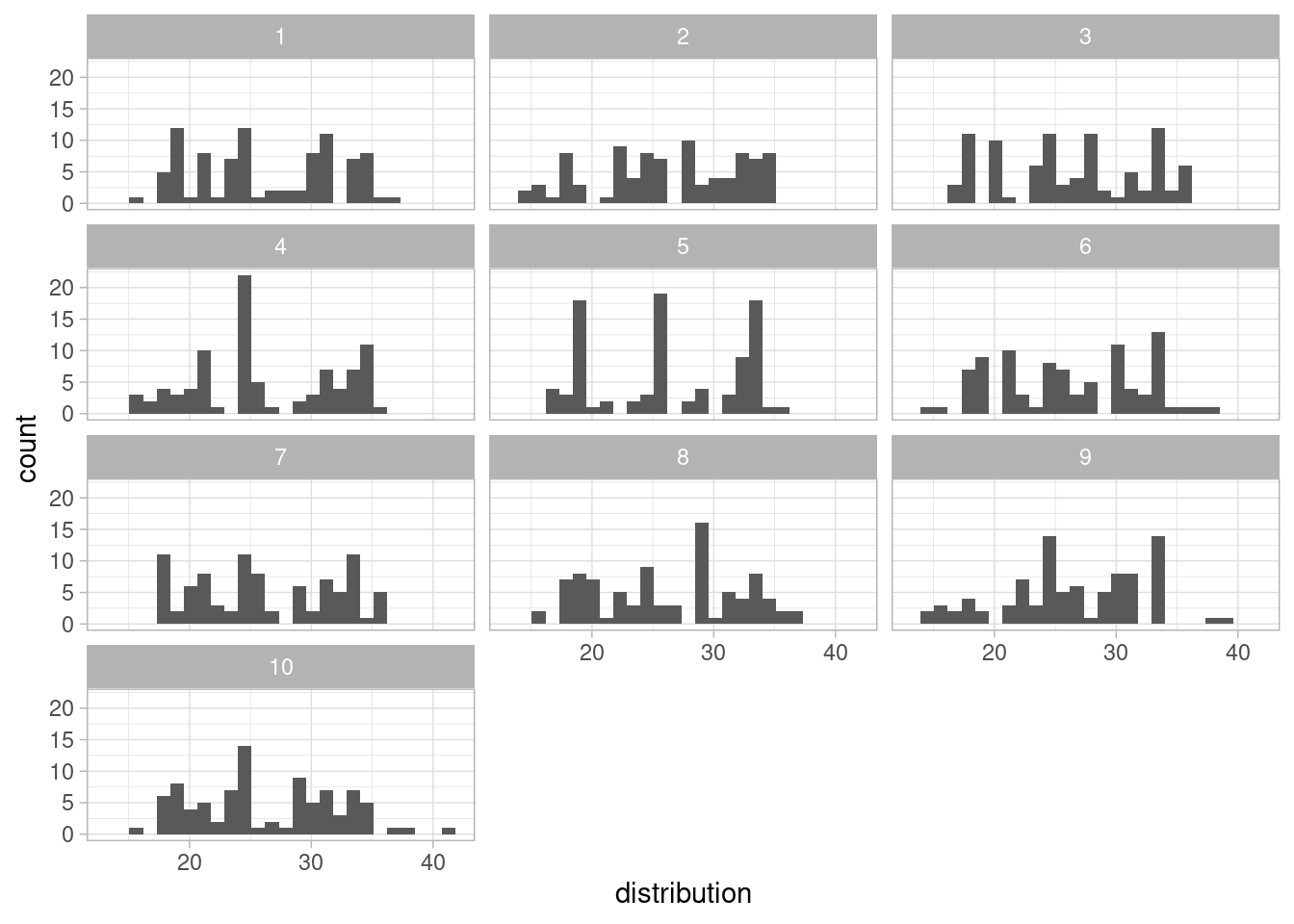
Wallrich, Lukas. 2023.
“Rsprite2: Identify Distributions That Match Reported Sample Parameters (SPRITE).” https://CRAN.R-project.org/package=rsprite2.
Wan, Xiang, Wenqian Wang, Jiming Liu, and Tiejun Tong. 2014.
“Estimating the Sample Mean and Standard Deviation from the Sample Size, Median, Range and/or Interquartile Range.” BMC Medical Research Methodology 14 (1).
https://doi.org/10.1186/1471-2288-14-135.
Westgate, Martin, and Eliza Grames. 2020.
“Synthesisr: Import, Assemble, and Deduplicate Bibliographic Datasets.” https://CRAN.R-project.org/package=synthesisr.
Westreich, D., and S. Greenland. 2013.
“The Table 2 Fallacy: Presenting and Interpreting Confounder and Modifier Coefficients.” American Journal of Epidemiology 177 (4): 292–98.
https://doi.org/10.1093/aje/kws412.
Wickham, Hadley. 2023.
“Stringr: Simple, Consistent Wrappers for Common String Operations.” https://CRAN.R-project.org/package=stringr.
Wickham, Hadley, Mara Averick, Jennifer Bryan, Winston Chang, Lucy D’Agostino McGowan, Romain François, Garrett Grolemund, et al. 2019.
“Welcome to the Tidyverse” 4: 1686.
https://doi.org/10.21105/joss.01686.
Wickham, Hadley, Jim Hester, Winston Chang, Kirill Müller, and Daniel Cook. 2021.
“Memoise: ’Memoisation’ of Functions.” https://CRAN.R-project.org/package=memoise.
Widhalm, Harald K., Alexander Draschl, Jannike Horns, Sebastian Rilk, Johannes Leitgeb, Stefan Hajdu, and Patrick Sadoghi. 2024.
“The Optimal Window for Reconstruction of the Anterior Cruciate Ligament (ACL) with Respect to Quadriceps Atrophies Lies Within 21 to 100 Days.” Edited by Filippo Migliorini.
PLOS ONE 19 (2): e0296943.
https://doi.org/10.1371/journal.pone.0296943.